Every time I teach anatomy, I get asked whether neck rolls/circles are safe to practice and teach. This movement has definitely made it into the top ten of the “thou shalt not” list!
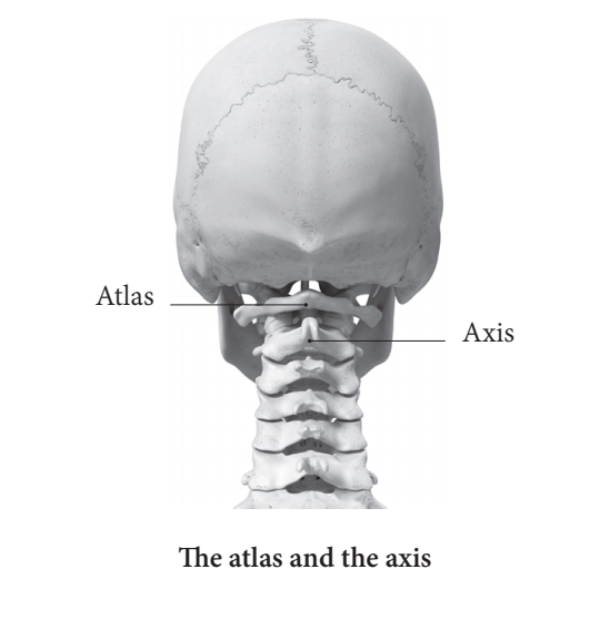
Let’s start by taking a quick look at the anatomy of our cervical spine. The craniovertebral junction (CVJ) is the complex relationship between the base of the skull, C1 and C2. This region houses vital neural and vascular structures while providing most of the cranial flexion, extension, and axial rotation. In fact, the range of movement at the junction exceeds that of any other region of the entire vertebral column. An intricate combination of bony and ligamentous supports allows for stability despite the large range of movement, while highly specialized muscles control fine movements in the CVJ. This region provides extensive three-dimensional placement of the head and neck, which is essential for optimal spatial orientation of the special senses (sight, hearing, smell, taste and balance). In summary – this region is designed to move a lot and for a very important reason!
Our bodies are so intelligent that if a particular movement was intrinsically bad for us, we simply wouldn’t have the option to perform it. Modern humans have been successfully evolving for the last 200,00 years – we wouldn’t have made it past year 1 if our cervical spines were inherently fragile!
One of the main reasons why neck pain and tension is so common is that we rarely move our cervical spine through its full range of motion. A study by Kim et al (2018) found that the occurrence of cervical area pain was higher amongst subjects who had a decreased CVJ and flexion motion. Unfortunately, fear-based statements encouraging us to not practice neck rolls will only lead people to move their necks even less.
Having said all of this, making large neck movements is not going to feel great or be a great idea for everyone. The key is to move slowly, with awareness and control, and to stay within a pain-free range.
It’s also important to mention cervical stenosis here, which is a narrowing of the spinal canal. Facet joint degenerative changes can result in enlargement of these small joints, which, in association with thickening of one of the spinal ligaments, can contribute to canal narrowing. In some cases, the narrowing can put pressure on the spinal cord. Lee et al (2007) estimated that cervical stenosis is present in nearly 5% of the adult population, approximately 7% of the population 50 years-of-age or older, and 9% of the population 70 years-of-age or older. A landmark study by Boden et al (1990) reported that 19% of patients with no symptoms had abnormal findings on scans of their cervical spine and that the prevalence increased with age. Of these asymptomatic subjects who were less than forty years-of-age, 4% had cervical stenosis. Of the subjects who were older than forty years-of-age, 20% had cervical stenosis. The cervical canal diameter is decreased with extension of the neck (Zeng et al 2016) and therefore a degree of caution may need to be taken here with students who have symptoms of cervical stenosis.
Join me for a short neck mobility practice:
References:
Boden, S., McCowin, P., Davis, D., Dina, T., Mark, A. and Wiesel, S. (1990) ‘Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation.’ J Bone Joint Surg Am 72, 1178-84.
Kim, D., Kim, C. and Son, S. (2018) ‘Neck Pain in Adults with Forward Head Posture: Effects of Craniovertebral Angle and Cervical Range of Motion.’ Osong Public Health and Research Perspectives 9, 6, 309–313.
Lee, M., Cassinelli, E., and Riew, D. (2007) ‘Prevalence of cervical spine stenosis: Anatomic study in cadavers.’ Journal Bone and Joint Surgery 89, 2, 376-380.
Zeng, C., Xiong, J., Wang, J. C., Inoue, H. et al. (2016) ‘The Evaluation and Observation of "Hidden" Hypertrophy of Cervical Ligamentum Flavum, Cervical Canal, and Related Factors Using Kinetic Magnetic Resonance Imaging.’ Global Spine Journal 6, 2, 155–163.