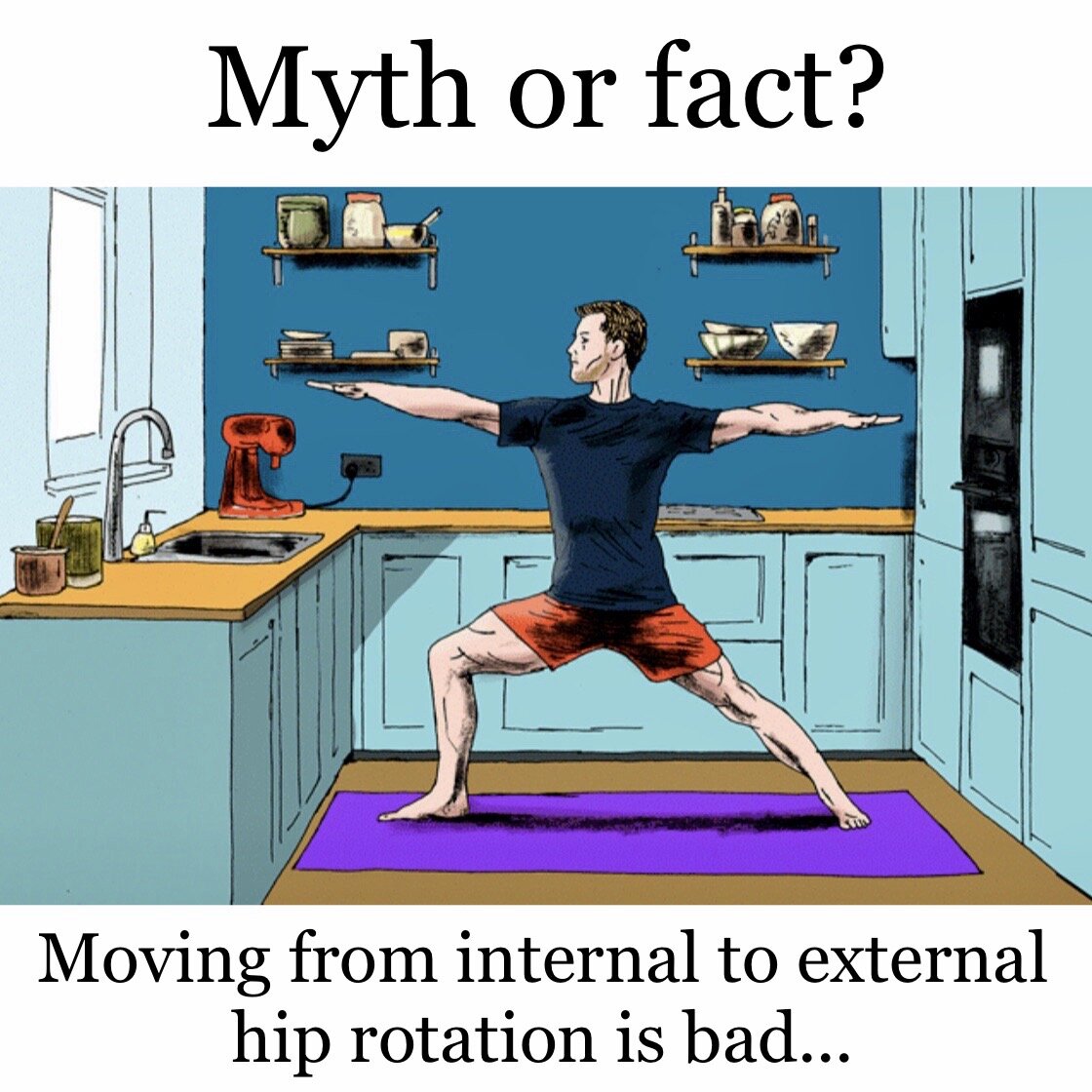
Yoga related hip pathologies have been a hot topic in the media recently and I personally have been asked about this topic every time I have taught hip joint anatomy. If you’re struggling to come up with examples in yoga where we move from one type of hip rotation to the other, think about transitioning from Warrior 3 (Virabhadrasana III) to Half Moon Pose (Ardha Chandrasana), or simply moving from Warrior 1 to Warrior 2 and vice versa.
My take on this somewhat controversial topic is that many of the correlations that are made between specific hip movements and specific hip pathologies are anecdotal, i.e. based on personal accounts rather than facts or research.
To the best of my knowledge there are no research studies that look at a potential link between specific hip movements and hip pathologies. While personal experience is valuable and often a great tool for learning, it can be easy to forget that in most cases our personal experience is personal, i.e. it can’t necessarily be related directly to other people. If you are a teacher and you find that these transitions don’t feel good for your body, it can be so easy to imagine that they are therefore not going to feel good for anyone else.
There is also the phenomenon of negative bias to take into account. If you experience something that you perceive as “negative” you are more likely to register that experience, dwell on it and relay it to others. We have all encountered this before. Think of a time when you received widespread praise for something but couldn’t stop fixating on the one piece of negative criticism that you received. As a yoga teacher you are more likely to head home ruminating about the student who left class early rather than the dozen students who told you how much they enjoyed the class. Therefore, the cases of “that yoga transition hurt my hip” are more likely to get discussed and shared than the cases of “oooh, my hip needed that!”
I often hear comments about specific movements or positions being bad for specific parts of the hip joint such as the labrum. The labrum of the hip joint is a fibro-cartilaginous rim attached to the margin of the acetabulum (hip socket). The exact function of the labrum is not fully understood but it may act to protect the edge of the acetabulum and fill up the irregularities of its surface. The labrum may also be involved in load distribution and lubrication within the joint (Ferguson et al 2003). The underlying cause of most hip pathologies including labral tears is not clearly understood. A study by Guanche and Sikka (2005) could not confirm an association between running and the development of labral tears or chondral lesions in the hip. A literature review by Groh and Herrera (2009) states that the prevalence of labral tears in patients with hip or groin pain has been reported to be 22–55%, however a study by Tresch et al (2017) reports that 57% of 20 to 50-year-olds with no hip pain will have cartilage deducts and/or labral tears. Groh and Herrera (2009) report that labral abnormalities have been found in patients without hip pain with the incidence increasing with age. This suggests that labral tears could be natural age-related changes.
Coming back to yoga, this highlights the importance of offering options and space to explore so that students can slowly begin to figure out what works best for them. At the end of the day it is really up to the individual to focus on how their hip joints feel in certain positions and during certain transitions. If moving from Warrior 3 (Virabhadrasana III) to Half Moon Pose (Ardha Chandrasana) with control feels okay, then this transition will most likely be fine for the weight-bearing hip joint. If in doubt, come to back to a neutral hip position before transitioning into the next asana. I am well aware that many students, particularly those who are hypermobile, have a much more challenging journey to discover what works best for them, but if we never give our students the opportunity to practice inquiry-based learning we are only stalling this journey rather than facilitating it.
References:
Ferguson, S., Bryant, J., Ganz, R. and Ito, K. (2003) ‘An in vitro investigation of the acetabular labral seal in hip joint mechanics.’ Journal of biomechanics 36, 171-8.
Groh, M. and Herrera, J. (2009) ‘A comprehensive review of hip labral tears.’ Curr Rev Musculoskelet Med 2, 105-117.
Guanche, C. and Sikka, R. (2005) ‘Acetabular Labral Tears with Underlying Chondromalacia: A Possible Association With High-Level Running.’ Arthroscopy 21, 5, 580–585.
Tresch, F., Dietrich, T., Pfirrmann, C. and Sutter, R. (2017) ‘Hip MRI: Prevalence of articular cartilage defects and labral tears in asymptomatic volunteers. A comparison with a matched population of patients with femoroacetabular impingement.’ J. Magn. Reson. Imaging 46, 440-451.