This blog post of an exclusive excerpt from my new book, The Physiology of Yoga.
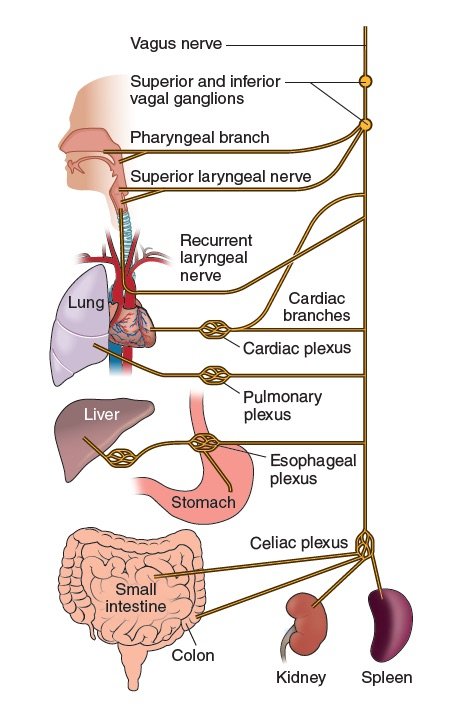
The parasympathetic nervous system (PSNS) works in opposition to the SNS to balance, calm, and restore the body. Its effect is often referred to as the rest-and-digest response. The vagus nerve is the 10th cranial nerve. It makes up about 75% of the PSNS. It is the longest cranial nerve in the body, extending from the head to the abdomen (the word vagus means wandering in Latin), and it provides parasympathetic input to most of the abdominal organs (except the adrenal glands and the descending colon), the muscles of the throat, the soft palate, the larynx, and part of the outer ear (figure 2.7).
It causes decreased heart rate, vasodilation of blood vessels, decreased respiratory rate, increased motility in the digestive tract, and release of digestive enzymes and insulin from the pancreas. Around 80% of the fibers of the vagus nerve are afferent, carrying sensory information to the central nervous system from our organs regarding how safe or unsafe we feel, therefore helping us to regulate our stress response.
So, how can we stimulate the PSNS? The key to this begins with a natural phenomenon occurring as part of our physiology: Parasympathetic nerves fire during expiration, contracting and stiffening airways to prevent collapse. Therefore, by lengthening our exhalation, we can directly target our PSNS. This is also why our heart rate naturally decreases with every exhalation (and naturally increases with every inhalation due to SNS activation). Singing, playing wind instruments, chanting, pranayama, and yoga can all stimulate the PSNS in this way.
A pilot study by Kalyani and colleagues (2011) concluded that chanting deactivated the limbic system, and the authors proposed that this was mediated by stimulation of the vagus nerve. Bernardi and colleagues (2001) found that recitation of the rosary prayers, and also of yoga mantras, slowed the respiratory rate to almost exactly six breaths per minute and enhanced parasympathetic activity. In addition to this, there is evidence that humming, through the action of lowering the pitch of your voice and creating resonance in the throat, can trigger the PSNS. A pilot study by Sujan and colleagues (2015) suggested that Bhramari pranayama (humming bee breath) increases parasympathetic activity.
There are many additional ways in which we can potentially stimulate the PSNS. When we are feeling stressed, our peripheral vision narrows so that we can focus on any imminent threats. By consciously focusing on our peripheral vision, we can potentially shift ourselves out of the stress response by triggering the PSNS. There is also preliminary evidence that acclimating to cold conditions lowers sympathetic activation and causes a shift toward increased parasympathetic activity (Mäkinen et al. 2008). This could be explored by regularly having cold showers. Research has even suggested that omega-3 fatty acids increase vagal tone and vagal activity (O’Keefe et al. 2006). A review by He and colleagues (2012) concluded that auricular (ear) acupuncture plays a role in increasing parasympathetic activity. Lu, Chen, and Kuo (2011) suggested that foot reflexology can increase vagal modulation, decrease sympathetic modulation, and lower blood pressure in healthy subjects and patients with coronary artery disease. Invited social engagement is also a key element. Porges (2011) has provided exciting insights into the way our autonomic nervous system unconsciously mediates social engagement, trust, and intimacy. Allowing ourselves to be truly vulnerable with others and accepting other people’s vulnerabilities can help us to feel safe and access our PSNS. A study by Kok and colleagues (2013) concluded that increased positive emotions, in turn, produced increases in vagal tone, an effect mediated by increased perceptions of social connections.
References:
Applegate, C., B. Kapp, M. Underwood, and C. McNall. 1983. “Autonomic and Somatomotor Effects of Amygdala Central N. Stimulation in Awake Rabbits.” Physiology and Behavior 31 (3): 353-630.
Barlow, D. 2002. Anxiety and Its Disorders: The Nature and Treatment of Anxiety and Panic. New York: Guilford Press.
Bernardia, L., A. Gabuttia, C. Portaa, and L. Spicuzza. 2001. “Slow Breathing Reduces Chemoreflex Response to Hypoxia and Hypercapnia and Increases Baroreflex Sensitivity.” Journal of Hypertension19:2221-2229.
He, W., X. Wang, H. Shi, H. Shang, L. Li, X. Jing, and B. Zhu. 2012. “Auricular Acupuncture and Vagal Regulation.” Evidence-Based Complementary and Alternative Medicine: eCAM 2012: 786839.
Iwata, J., K. Chida, and J. LeDoux. 1987. “Cardiovascular Responses Elicited by Stimulation of Neurons in the Central Amygdaloid Nucleus in Awake but Not Anesthetized Rats Resemble Conditioned Emotional Responses.” Brain Research 418 (1): 183-188.
Kalyani, B., G. Venkatasubramanian, R. Arasappa, N. Rao, S. Kalmady, R. Behere, H. Rao, M. Vasudev, and B. Gangadhar. 2011. “Neurohemodynamic Correlates of ‘OM’ Chanting: A Pilot Functional Magnetic Resonance Imaging Study.” International Journal of Yoga 4 (1): 3-6.
Kok, B., K. Coffey, M. Cohn, L. Catalino, T. Vacharkulksemsuk, S. Algoe, M. Brantley, and B. Fredrickson 2013. “How Positive Emotions Build Physical Health: Perceived Positive Social Connections Account for the Upward Spiral Between Positive Emotions and Vagal Tone.” Psychological Science 24 (7): 1123-1132.
Lu, W., G. Chen, and C. Kuo. 2011. “Foot Reflexology Can Increase Vagal Modulation, Decrease Sympathetic Modulation, and Lower Blood Pressure in Healthy Subjects and Patients With Coronary Artery Disease.” Alternative Therapies in Health and Medicine 17 (4): 8-14.
Mäkinen, T., M. Mäntysaari, T. Pääkkönen, J. Jokelainen, L. Palinkas, J. Hassi, J. Leppäluoto, K. Tahvanainen, and H. Rintamäki. 2008. “Autonomic Nervous Function During Whole-Body Cold Exposure Before and After Cold Acclimation.” Aviation, Space, and Environmental Medicine 79 (9): 875-882.
McCorry, L. 2007. “Physiology of the Autonomic Nervous System.” American Journal of Pharmaceutical Education 71 (4): 78.
O’Keefe, J., H. Abuissa, A. Sastre, D. Steinhaus, and W. Harris. 2006. “Effects of Omega-3 Fatty Acids on Resting Heart Rate, Heart Rate Recovery After Exercise, and Heart Rate Variability in Men With Healed Myocardial Infarctions and Depressed Ejection Fractions.” American Journal of Cardiology 97 (8): 1127-1130.
Porges, S. 2011. The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-Regulation. New York: Norton.
Schmidt, N., J. Richey, J. Zvolensky, and J. Maner. 2008. “Exploring Human Freeze Responses to a Threat Stressor.” Journal of Behavior Therapy and Experimental Psychiatry 39 (3): 292-304.
Sujan, M., K. Deepika, S. Mulakur, A. John, and T. Sathyaprabha. 2015. “Effect of Bhramari Pranayama (Humming Bee Breath) on Heart Rate Variability and Hemodynamic—A Pilot Study.” Autonomic Neuroscience 192 (82): 1